When young people turn 18, a lot happens. Adult responsibilities and decisions can feel scary and confusing for the unprepared. Becoming responsible for medical care is part of growing up, and that process is so critical that there’s a specific name for it: healthcare transition.
For example, at age 18 a young adult is responsible to sign official paperwork to authorize procedures or therapies. They must sign documents to say who can look at their medical records, talk to their doctors, or come to an appointment with them. Those rules are part of HIPAA, which stands for the Health Insurance Portability and Accountability Act. HIPAA is a federal law that protects confidentiality, regardless of disability.
In this video, young adults living with various disability and medical conditions talk about their journeys in the adult healthcare system. They talk about how they make decisions and how they ask for help. Their ability to explain their needs, make decisions, and speak up for themselves is called self-advocacy. Take a look and listen to what they have to say in their own words!
For more information and resources around healthcare transition and self-advocacy, follow these links to the Family to Family Health Information website.
PAVE also has a Healthcare In Transition article that will give you detailed information for individuals transitioning from Pediatric (Children’s) to adult health care including information on health insurance and providers.
Another place for information is the Informing Families website, which includes a section called got transition.
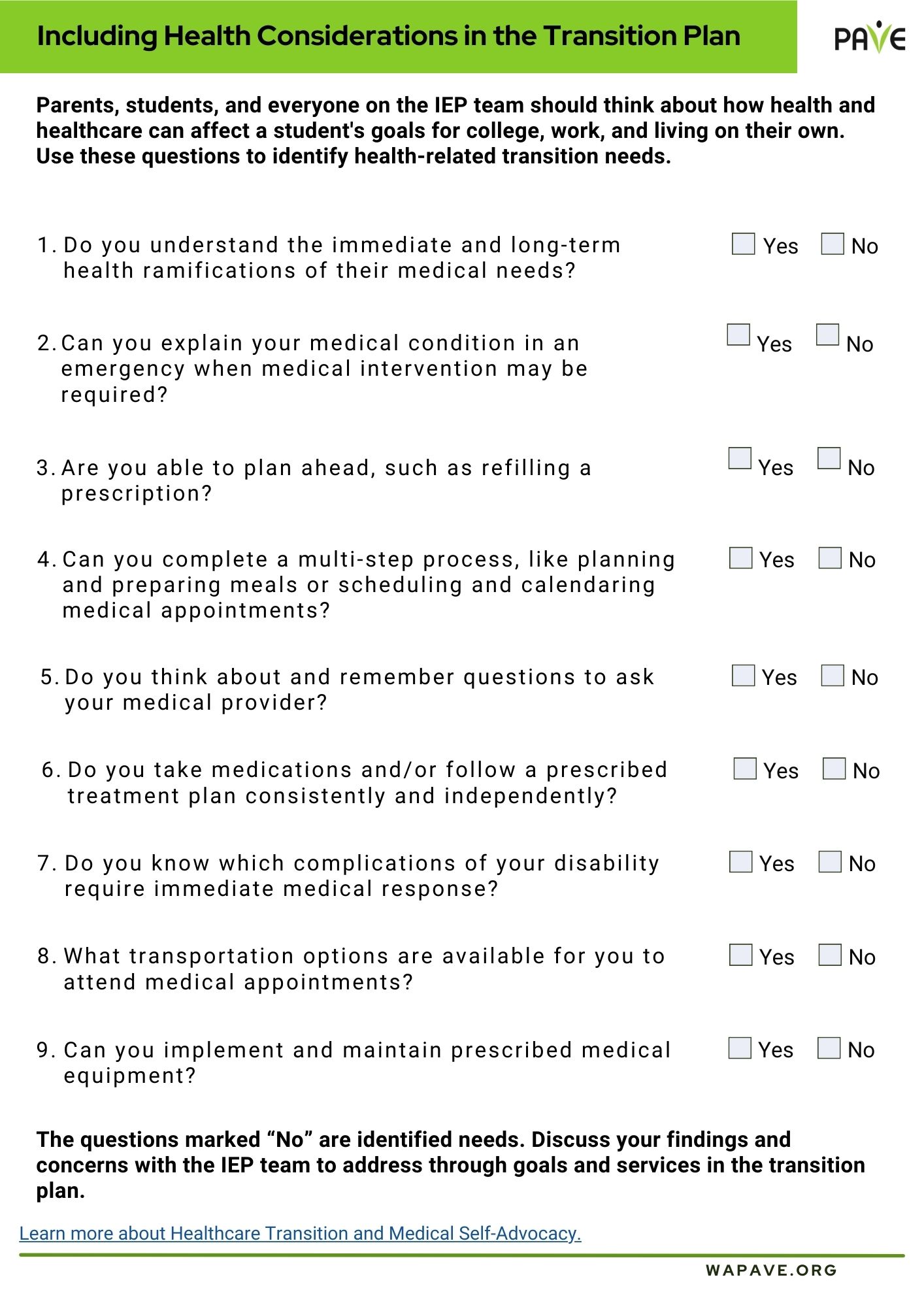
Including Health Considerations in the Transition Plan
Parents, Students, and everyone on the IEP team should think about how health and healthcare can affect a student’s goals for college, work and living on their own. PAVE has made a fillable form that you can download when starting to think about this area in transition.