When your child is impacted by chronic healthcare needs or disability it can be very important to learn to talk with the healthcare professionals that work with your child. Having a relationship that allows for respect and understanding makes it easier for families, the patient (if they are older), and the doctor or specialist to communicate concerns and changes.
This article covers how preparation for a medical visit helps with communication, three key Communication Actions to follow with health providers, removing communication barriers and issues, communication styles, and introductions to youth health care transition and medical homes.
A Brief Overview
- Respectful, two-way communication is a baseline for your child or youth’s best medical care.
- Preparing yourself (and your child or youth) for a medical visit helps get the most from a conversation with your medical professional and supports successful communication for the future.
- While there may be times when there are differences in ideas or understanding between you and your child’s medical team, communicating based on your knowledge as a parent can help the team gain a broader perspective.
The good news is that most communication difficulties can be solved! This article has many examples of how to do it. - The way parents communicate can help get the attention of your child’s medical provider.
- Medical Homes are designed to make communication and working as a team easier. This article includes a brief explanation of medical homes and links to more information.
- Children reach an age when they are allowed, by law, to make medical decisions for themselves. This article introduces the concept of health care transition and gives resources for more information on this important topic.
Introduction
When your child is impacted by chronic healthcare needs or disability it can be very important to learn to talk with the healthcare professionals that work with your child. Having a relationship that allows for respect and understanding makes it easier for families, the patient (if they are older), and the doctor or specialist to communicate concerns and changes.
Preparation Helps
Knowing what might happen during a medical visit is one way to prepare yourself to be a good communicator. Having a general idea of what a doctor or other health care provider wants to learn during an appointment is also a good first step.
The US Department of Health and Human Services has web pages for parents called “Make the Most of Your Child’s Visit to the Doctor”. They are on the MyHealthFinder site on the “Regular Checkups” page.
These resources are geared to parents of children without disabilities, but since accidents, sickness, developmental or behavioral health problems can occur at many points in a child’s life, they may be helpful as a place to begin. Each set of web pages has an age range, and the information is specifically for parents of children of those ages.
- The “Take Action” page in each two-page section has tips on preparing for the visit, including questions the nurse or doctor might ask, and questions you might wish to discuss.
- The examples include items you might not have thought about, so they can help you think about discussing a broad range of topics during the visit.
Communication difficulties (barriers) and how to solve them
Sometimes parents may find it difficult to speak up with doctors, nurses, and other health care providers because:
- Your child may have been born with a medical condition, and you as parents have been viewing health care providers as “the experts” since your child’s birth.
- If you, as a parent, grew up with the custom of taking a “professional’s” advice even if you have questions or you don’t believe their advice will work for your child.
- You don’t know enough about your child’s development or condition to know if the proposed treatment is a good idea for your child.
- You may be nervous about challenging a health care provider’s advice or treatment plan because you worry it might affect your child’s care.
Dr. Rachel Bies is a pediatrician in Minnesota, and she wrote about parents not feeling heard in a blog post. She writes there “is a balance between what the provider feels is in the best medical interest of the child and what the parent feels is in the best interest of their child and family. We share the common goal of the health of the child but may have different ideas about how to achieve that goal.” (emphasis added).
If a parent does not feel they are being heard by their child’s pediatrician or health care provider, she asks parents to think about what might be causing communication barriers. Some common barriers in medical settings include:
- Language differences
- Too much use of medical terminology
- Time limits on an appointment
- Cultural differences
- Different expectations for the visit
To get around these barriers, you can take some or all these actions:
- You can ask for an interpreter, and for medical information sheets to be translated or available in your preferred language.
- You can bring along another person to take notes and ask questions you forget to ask. (Dr. Bies mentions that people tend to only remember about 50% of discussions in a healthcare visit). You can expect an after-visit summary or a handout to help remember important information.
- Ask for medical terminology be explained.
- You can tell the health care provider about any cultural practices which are related to your child’s health or care.
- Ask who you should call or email if you have follow-up questions.
- If time is limited, are there ways to discuss less urgent matters with an appropriate member of the medical team?
- For instance, some practices and clinics have message phone lines or emails so patients or parents and guardians can ask questions and get answers from a team member less pressed for time, such as a nurse or nurse practitioner. Doctors, and particularly specialists, may be the most tightly scheduled staff in a practice or clinic. Another option may be to book a telehealth follow-up appointment for your questions, if covered on your health plan.
- To help make your expectations clear, let the health care provider or team know up front, if possible.
- Almost all advice about preparing for a medical appointment tells patients (or parents) to bring a list of current questions and concerns. Some practices have a document that patients or parents fill out in the waiting room “What brings you here today?” Rather than trying to transfer your list of questions to the document, bring a copy of your questions and a paper clip, and when you turn the form in, ask for your list to be stapled to the form so all the information gets added to your child’s record.
Even when there are no obvious communication barriers, you can ask yourself:
- “Are my opinions and knowledge of day-to-day changes being noted? What does the health care provider say about them?”
- In situations where you believe there is a need for action, ask yourself “Major changes are happening with my child, and I have brought them to the attention of the health care provider or team. Has anyone in the practice (clinic, hospital) been providing resources to help with these changes? Have I or my child been referred to additional health care providers or resources?”
If you can’t answer “yes” to these questions, it might be time to look for a different health care provider.
Most people are somewhat limited in their choice of providers because of their particular health insurance. This is true whether you are on publicly funded health plans like Medicaid (Apple Health and CHIP) or TRICARE, private insurance through an employer, or Affordable Care Act (ACA or Obamacare) plans through Washington Healthplanfinder.
Another limitation may be the limited choice of health care providers in your area.
These are two important reasons to first try different ways to communicate with your child’s health care team, if your first attempts do not seem to work.
Three Key Communications Actions and Communication Styles
In a short YouTube video from Seattle Children’s Hospital, Lisa Peters, MN, RN talks about doctor-parent communication about pain management. The ideas in the video work for any situation where parents need to communicate with health care providers.
The three key Communication Actions are:
- Speak Up
- Partner
- Advocate
Ms. Peters points out that “at any time, you have the right to stop and make a change in [your child’s] plan if it’s not working for your child.”
PAVE’s article “Self-Advocacy: Becoming an Active Member in Your Community” is helpful for anyone who wishes to communicate in ways that result in partnering with healthcare professionals while advocating for their child.
Here are some tips from the article. The wording has been changed a bit to make it more about parents, children, and health care settings.
- Learn about the topic you are speaking about (your child’s condition or disability).
- Actively listen to the other person and ask if you don’t understand something (like a medical term).
- Try to see the other person’s point of view. Most health care providers want to partner with patients and parents. You have the right to ask why they recommend a particular plan or treatment, and you can also explain your point of view:
“This plan means Tommy needs to be in the hospital for multiple procedures. Can you explain a bit more why you want the procedures to happen very close together?” - Express your feelings clearly, calmly, and assertively, without being aggressive or disrespectful.
- What is an assertive communication style? A page at Nemours TeensHealth offers many easy-to-understand tips, and examples of how to achieve an assertive style of communication and advocacy for both teens and adults. They write “Assertiveness is a healthy way of communicating. It’s the ability to speak up for ourselves in a way that is honest and respectful.” (emphasis added).
Medical Homes can help with communication
A medical home is a communication hub designed to focus on providing better medical communication with the patient’s family and medical and school medical IEP providers. The hub is a central communication manager where all members involved in the patient’s case can call to update medications, medical notes, upcoming appointments, and the family can call to contact doctors in an emergency or leave questions. The parent or guardian of the patient can select the hub. Possible hubs could be a primary care provider, a specialist, a medical case manager, DDA case manager or the parent or guardian. PAVE has a video and article which helps to define a medical home. The article offers questions to help you decide if your family may need to create a medical home. Washington State Medical Home Partnership Project has a website full of resources to help with medical homes, including The ABC’s of Medical Homes.
Health Care Transitions
In Washington State, children reach the age of majority for medical care at 18, which means they can get healthcare services in Washington State without an adult’s permission. It’s also a common age to move from the care of a pediatrician to a medical provider who treats adults. Preparing for this change is called “transition for medical care.” Just like the similar process for life after high school, “transition for medical care” begins much earlier than 18, and usually involves help from parents or guardians and the current medical providers. This “transition” is especially important to youth and young adults with a disability, as part of their preparation to take charge of their life as an adult.
Important to know: the “age of medical majority” for teens is not always age 18. For certain types of medical treatment or testing, children aged 13 through 17 “can make their own decision to get birth control, seek mental health treatment, and get tested for sexually transmitted infections (STIs) and more” based on Washington State’s privacy laws. Adults 18 and over who are under legal situations like guardianship may not always be able to make healthcare decisions for themselves.
Information on healthcare permissions, privacy, guardianship and many other legal topics can be found at WashingtonLawHelp.org.
Many parents prepare their children to transition to adult healthcare when they are small, just by preparing them for medical appointments. Imaginative play of the child being the doctor and the parent being the patient re-enacting the scene of a doctor’s visit starts to prepare children for how to interact with healthcare providers. As the child gets older, we talk to them prior to a doctor’s visit about why we are going and ask if they have any questions we are building on the foundation.
Teens are encouraged to learn about their medical and other allergies, what their health or disability condition is, what medications they take and the dosages. Gottransition.org has resources for parents outlining the stages and goals of the transition process. All stages and goals are flexible based on each youth’s ability levels, healthcare needs and personal needs, this is a guideline. Gottransition.org has resources to assist youth in discussing their concerns about transitioning to adult health care with their doctor and an electronic means of keeping track of their health ID card.
While transitioning from pediatric health care to adult health care, teenagers are developing their advocacy skills with their parents and their peers. Now, teenagers are having to learn how to advocate for themselves in an environment that can be uncomfortable at times. A short video presented by the University of Michigan’s website Michigan Medicine is Teen Self-Advocacy: How To Be Your Own Healthcare Advocate. It provides tips on self-advocacy in the doctor’s office. Teens may find electronic resources useful advocacy tools to plan their doctor’s visits.
The Academy of American Pediatrics provides a tool to assist with preparing for a doctor’s appointment, Well Visit Planner and Patient Question Builder app. (Scroll down to the middle of the page.)
Before using any phone or computer app, AAP advises that users check that no information is collected or saved, and the app does not sell any information to third parties.
Parents can struggle with letting go of control over the health care of a youth with complex medical needs or a disability. Managing their child’s health care needs has been a major factor in their lives for as long as they can remember. This anxiety can create tension between teenagers and parents. Michigan Medicine presents a video showing a group of parents as they discuss their different parenting experiences through this transition period. Each experience is unique as each child is unique. Parents are learning to step back during doctor’s appointments and let their teenager speak to the doctor, asking questions about the doctor’s recommendations and ensuring that they understand the information presented. You may want to watch this video with your child who is transitioning to adult health care as a conversation starter about your feelings and their feelings about this transition period.
A teenager needs to know their rights to privacy. A downloadable pdf from the Adolescent Health Initiative at Michigan Medicine outlines the privacy rights of a teenager with their healthcare professional. At all times patients are encouraged to talk to their medical professionals if they have any questions about confidentiality. Sharing this privacy document with your teenage child lets them know that you support their own healthcare communication and advocacy with their current and future health care providers.
Health Information and Your Privacy is a resource to help adults and minors keep their privacy by having their insurance provider send any communications or documents
Additional information on Health Care Transition
- When is it Time for me to Transition to Adult Doctors?
- What Can I Expect When Transitioning From Pediatric Care to Adult Doctors?
- What Questions Should I Ask While Transitioning From Pediatric to Adult Doctors
- What Young Adults with Disabilities Have to say About Health Care Transitions and Medical Self-Advocacy (video)
- Transition from Child Based to Adult Based Services in Behavioral Health
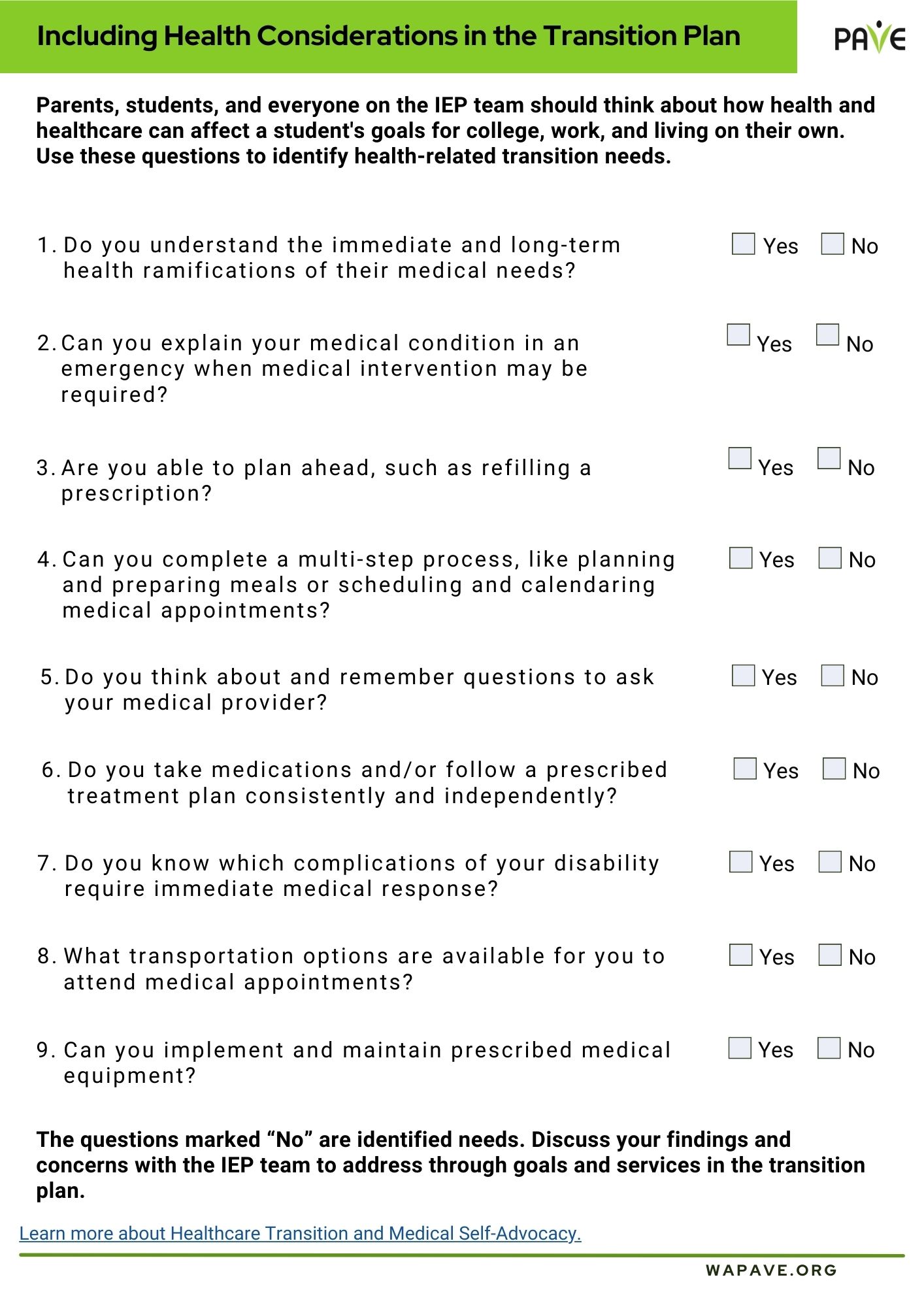
- Healthcare Transition and Medical Self-Advocacy
- Healthcare in Transition