A Brief Overview
- WISe behavioral healthcare teams serve children and youth 20 or younger whose conditions are too severe to benefit appropriately from regular visits to a community clinician and/or therapist.
- To qualify for WISe, the young person must be eligible for Apple Health, which is the public health program for Washington State. WAC 182-505-0210 describes Apple Health eligibility standards.
- WISe was created as a response to the T.R. et al. lawsuit, settled in 2013.
- Different agencies manage WISe programs in various regions of the state. The Health Care Authority manages a downloadable list of WISe agencies, organized by county. Families can contact their area agency by calling the phone number on this referral list.
- Read on for various places families might seek solidarity and support. One option is Family, Youth, and System Partner Round Table (FYSPRT), which is a network of groups that meet to discuss what’s working/not working in behavioral healthcare systems in their communities.
Full Article
Children and youth with intensive needs related to behavioral health may be eligible for services from a statewide program called WISe–Wraparound with Intensive Services. A WISe team includes various clinical and professional staff and certified peers, who may support the emotional needs of family members.
WISe services are provided in the community—outpatient—for children and youth 20 or younger who are eligible for public insurance, called Apple Health in Washington State. To be assigned to a WISe team, the young person must demonstrate a need for services that are more intensive than what is provided from regular visits to a community clinician and/or therapist.
What does behavioral health mean?
Behavioral health is a broad term describing services for people with conditions based in the brain that impact their behavior. Bipolar disorder, schizophrenia, and substance use disorder (SUD) are examples of severe behavioral health conditions impacting some adults and young people.
Other childhood conditions are many and varied, and not everyone uses the same terms for the same symptoms. The Child Mind Institute is a place for information about childhood symptoms, diagnoses, and options for treatment and support.
Some developmental conditions, such as autism, are considered behavioral health conditions when symptoms have a significant impact on behavior. A person with a complicated behavioral health condition may have impacts in multiple areas and may be given a “dual diagnosis.”
Who is eligible for WISe services?
WISe services are for children and youth until their 21st birthday. WISe is only approved if the patient has used other, less intensive therapies, with little to no improvement. Once approved for services, a young person may spend time on an “interest list,” receiving limited support, before a full team is formed to serve them.
The young person is evaluated with a Child and Adolescent Needs and Strengths (CANS) intensive mental health screening tool, called the CANS-SCREEN.
Five core areas are evaluated:
- Life functioning
- Behavioral and emotional needs
- Risk behaviors
- Caregiver resources and needs
- Diagnosis and prognosis
According to the CANS-SCREEN, “The care provider, along with the child/youth and family as well as other stakeholders, gives a number rating to each of these items. These ratings help the provider, child/youth and family understand where intensive or immediate action is most needed, and also where a child/youth has assets that could be a major part of the treatment or service plan.”
WISe requires public health insurance eligibility
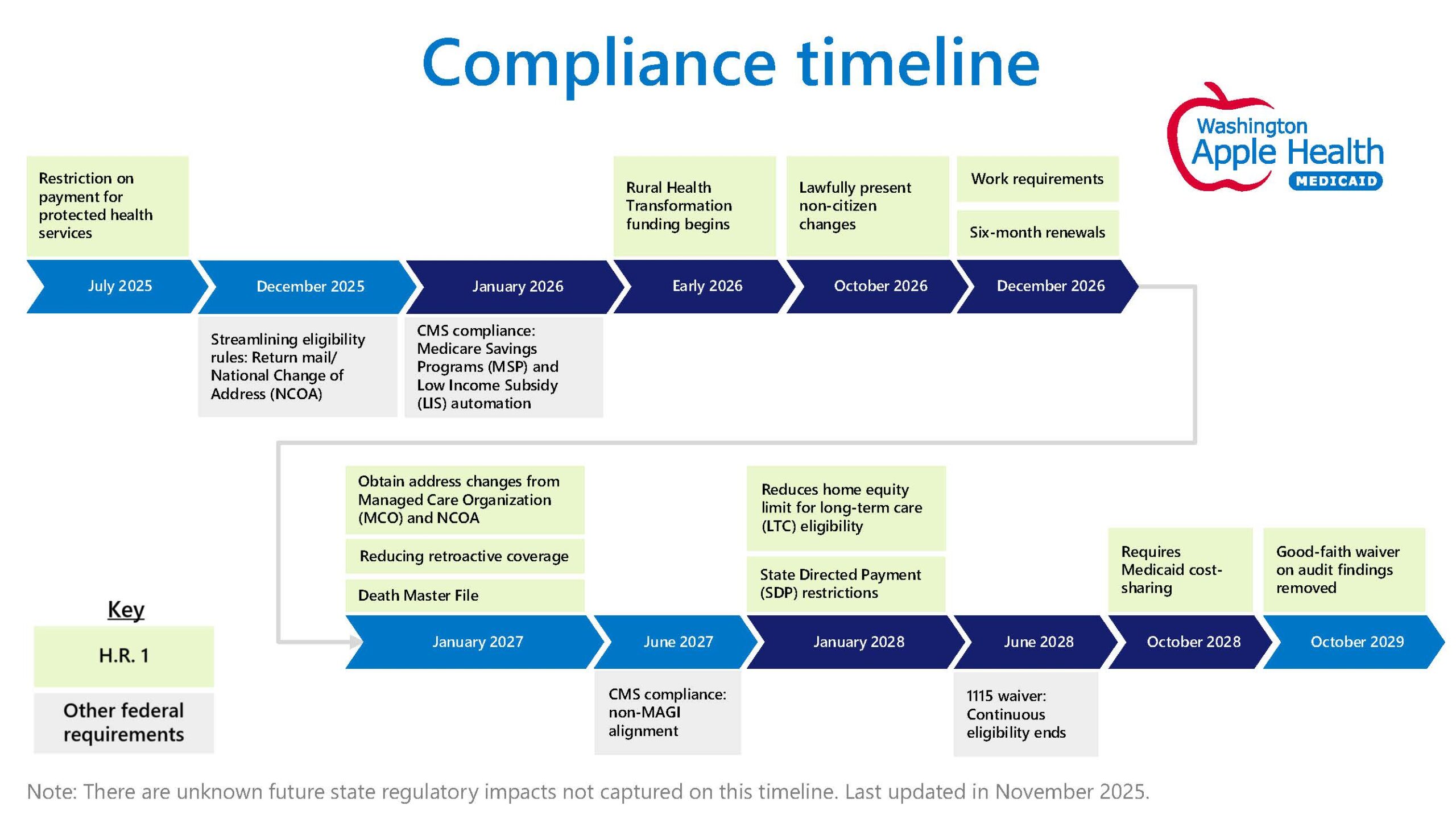
In addition to meeting criteria based on their symptoms, a young person must be eligible for Apple Health, which is the name for public health insurance in Washington State. The Washington Administrative Code (WAC 182-505-0210) describes Apple Health eligibility standards for children.
Apple Health is most often administered by Managed Care Organizations (MCOs). In 2022, plans are provided by Amerigroup, Community Health Plan of Washington (CHPW), Coordinated Care, Molina, and United Healthcare. Families can request case management from their MCO to help them navigate and understand healthcare options available to them.
An MCO care coordinator/case manager commonly is the person who refers a young person into WISe, although referrals also can be made by the family, a provider, a county health agency, or someone else with knowledge of the circumstances.
Different agencies manage WISe programs in various regions of the state. The Health Care Authority manages a downloadable list of WISe agencies, organized by county. Families can contact their area agency by calling the phone number on this referral list.
Who is on the WISe team?
Team members include:
- Natural supports (family, friends, religious leaders…)
- A Care Coordinator (who oversees clinical aspects of the case)
- Therapist
- Professionals (clinicians/prescriber if needed, Child Protective Services, probation officers and others who are relevant)
- Certified peer support specialist
- Others upon request (youth peer, school staff…)
The clinical group creates a Team Vision Statement, explaining what they plan to achieve and how they will accomplish it through collaborative work. The family also creates a Vision Statement, showing what strengths they would like to build in their family and what tools they need to make their goals possible.
WISe requires family engagement
The time commitment for WISe is significant. Clinicians engage with the whole household on topics related to school, health, work, relationships, home organization, and more.
WISe publishes data about its service delivery. According to January 2021 Service Intensity Estimates, an average family spends 10 or more hours per week engaged with WISe services. This could be much higher, especially in the beginning. Parents/Caregivers are offered therapy sessions and opportunities to engage with parent peers.
WISe clinicians are responsible to integrate their work to fit with a family’s schedule, often seeking creative ways to tuck sessions into already busy days. For example, a clinician describes a day when they picked up a child at school and conducted a session in the car while driving the child to their next activity. After work, parent met with the clinician while the adults watched the child swim.
Family experiences with WISe are varied. Some say WISe created a critical turning point that enabled family survival. Others cite high staff turnover as a barrier to ideal therapeutic outcomes. The program is most effective with buy-in from the young person and their caregivers and when services are provided to match family needs and schedules.
Does my child have to agree to WISe services?
WISe is a voluntary program. Families may be able to motivate their child to participate by getting services started through Family Initiated Treatment (FIT). FIT was established as a pathway to treatment for youth 13-17 when Washington passed the Adolescent Behavioral Health Care Access Act in 2019. A parent/caregiver can initiate outpatient services to attempt to get the youth to engage. If after 12 visits (within 3 months) the youth is still unwilling to engage with the treatment, the family must end services. They have the option to engage a different provider to try FIT again.
What if WISe isn’t enough?
The WISe program is the most intensive outpatient program that the state offers. If services don’t seem to be working, the family might check the WISe Service Delivery, Policy, Procedure and Resource Manual to see whether there is more the program could be doing. The family also might check if the child could get additional services from another agency to complement the work with WISe. For example, service providers from a special education program at school or from the Developmental Disabilities Administration (DDA) can collaborate with a WISe team.
If a child needs inpatient services, they may be eligible for a referral into the Children’s Long-term Inpatient Program (CLIP). Children placed on a waiting list for CLIP often receive ongoing services from WISe. PAVE provides an article: Children’s Long-Term Inpatient Program (CLIP) Provides Residential Psychiatric Treatment.
History, Advocacy, and Family Support
WISe was created as a response to the T.R. et al. lawsuit, settled in 2013. The class-action lawsuit named ten plaintiffs who were denied treatment for schizophrenia, depression, bipolar disorder, and other serious psychiatric conditions. Most were institutionalized repeatedly and for extended periods, despite recommendations by therapists and case workers that they return home and receive services in their homes and local communities.
Disability Rights Washington (DRW) provided attorney support for the settlement of the T.R. et al. lawsuit. DRW is monitoring current issues related to children being underserved through WISe and encourages families with concerns to contact attorney Susan Kas: susank@dr-wa.org.
Another result of the legal settlement was a statewide network of stakeholders who meet regularly to discuss what works/doesn’t work within the behavioral health system for youth. That network is called Family, Youth, and System Partner Round Table (FYSPRT). Regional FYSPRTs report to a statewide FYSPRT to share input for system improvement. Regional groups are a hub for family networking and emotional support in addition to serving as a place to engage with community health providers, insurance case managers, and other professionals. Some FYSPRTs have distinct groups for young people to meet and support one another. Many FYSPRT groups use online meeting platforms due to the pandemic.
Another place for families engaged in behavioral health services to network is Washington State Community Connections (WSCC), which sponsors an annual family training weekend, manages an SUD Family Navigator training, and offers a variety of ways for families to share their experiences and support one another. WSCC in 2022 is engaged in work to help build a statewide website to help families navigate behavioral health services across systems. Stay tuned!
Families can get direct support from A Common Voice, a statewide non-profit staffed with Parent Support Specialists who have lived experience parenting a child with challenging behavioral health conditions. The program offers virtual support groups and 1:1 help. A Common Voice is part of the Center of Parent Excellence (COPE), managed by the state’s Health Care Authority. The COPE project website provides a schedule of support group meetings and contact information for regional lead parent support specialists.
An informal place to connect with other families is a Facebook group called Healthy Minds Healthy Futures. Advocates in this group initiated work for an interactive website for parents and are engaged in a push for HB 1800 to expand behavioral health services for minors statewide.
Families wanting to advocate for system change can participate in meetings of the Children and Youth Behavioral Health Work Group (CYBHWG). The work group was created in 2016 by the Legislature (HB 2439) to promote system improvement. CYBHWG supports several advisory groups, including one for Student Behavioral Health and Suicide Prevention. The work groups include representatives from the Legislature, state agencies, health care providers, tribal governments, community health services, and other organizations, as well as parents of children and youth who have received services. Meetings include opportunities for public comment. Meeting schedules and reports are posted on the Health Care Authority (HCA) website.
Parity laws, thoughtful language, stopping stigma
Keep in mind that a healthy mind is part of a healthy body, and U.S. laws protect parity for all illness conditions. Despite those protections, discrimination and stigma are commonly discussed within behavioral healthcare systems. Here are a few tips and considerations to help reduce stigma:
- All behaviors start in the brain, so an impairment that impacts the brain is going to affect behavior. Some behaviors are not a person’s fault; that’s why they need treatment, support, and services.
- Specific person-first language can help reduce stigma. For example, instead of calling someone bipolar or schizophrenic, say they are a person with bipolar disorder or schizophrenia.
- An exception to person-first language is in the autism community, which has collectively agreed to use the term “autistic” to describe someone on the spectrum.
- Saying that someone has “behavioral health,” or “mental health” does not describe their condition or what they need help with. Everyone has mental health! A better choice is to describe the condition/concern and the need for help: “This youth’s schizophrenia is impacting every aspect of life, and they need a range of services and treatments to recover and move forward with their life plans.”
- A person who dies from suicide did not commit a crime, so the word “commit” is inappropriate to use when discussing suicide.
For additional information on related topics, including areas where behavioral health impacts school, see PAVE’s article: Mental Health Education and Support at School can be Critical